Sally Ezra/CDC
The Imperfect Attempt to Chase Ebola
Scientists are using computer models to predict the outbreak's next moves, but they can't account for human behavior.
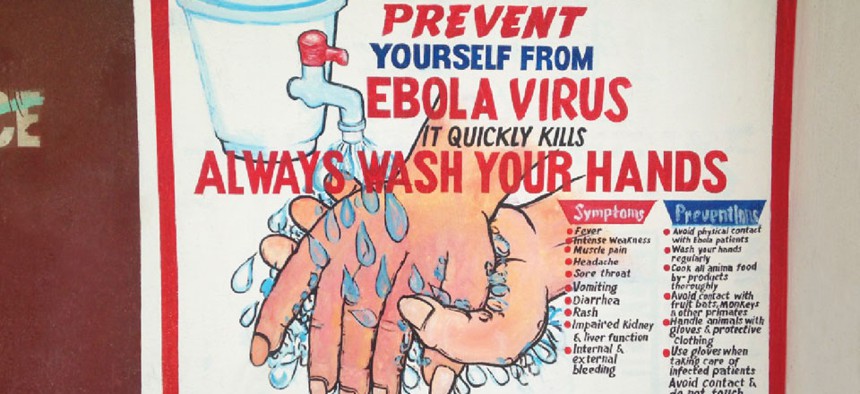
In the early stages of the Ebola outbreak, the World Health Organization, Doctors Without Borders and other aid organizations concentrated their efforts on the ground. They tried to convince patients to go to hospitals or let aid workers set up quarantine areas in their homes. Unfortunately, these and other interventions did little to slow the outbreak. According to the WHO, the number of cases has nearly doubled in the last three weeks, prompting Sierra Leone’s government to enforce a three-day lockdown over the weekend.
On September 17, WHO director general Margaret Chan said there are now at least 5,357 reported cases, including 2,630 deaths, in Guinea, Sierra Leone, Liberia, Nigeria, and Senegal. "None of us experienced in containing outbreaks has ever seen, in our lifetimes, an emergency on this scale," she said. She has previously said the numbers are an underestimate, as there are many unreported cases. On September 16, the U.S. Centers for Disease Control and Prevention called the outbreak the world’s first Ebola epidemic.
As the speed of this outbreak increased, experts planning the response started relying more heavily on computer models, says Dr. Martin Meltzer. Meltzer is a senior health economist at the CDC, where he leads the Health Economics and Modeling Unit. On August 4, Meltzer started building the CDC’s Ebola models, called EbolaResponse.
Right now, the goal is to use the models to understand how to get the rate of transmission to an average of less than one infected person per infectious person, Meltzer told me. This is what has worked in stifling previous infectious disease outbreaks.
His first step is plotting the number of cases, to determine how many more will emerge if the outbreak continues at its current rate. According to a paper he published today in the CDC’s Morbidity and Mortality Weekly Report, the model shows that there will be 8,000 cases in Sierra Leone and Liberia by September 30 if there is no significant increase in the impact of health interventions. When the CDC corrects for potential unreported cases, the number spikes to 21,000 cases by September 30. Looking farther ahead, the numbers are shocking: By January 2015, Sierra Leone and Liberia could have 550,000 cases, or 1.4 million if corrected for underreporting.
Meltzer then uses the model to understand how to stop this from happening by testing different hypothetical situations. Experiments with the models have suggested that roughly 70 percent of patients would need to be in an effective quarantine setting, either at a hospital, Ebola treatment unit, at home, or through a safe burial, in order to bring the outbreak under control. Approximately 10 percent of patients are currently in these safe settings. If the goal of 70 percent is reached by December 22, the epidemic in Liberia and Sierra Leone “would almost be ended by January 20, 2015,” Meltzer wrote.
Even then, there are things that the model cannot account for. “Appreciate that not all hospitals/Ebola treatment units and certainly not all households with a patient ‘at home with effective quarantine/ isolation’ will be entirely secure,” Meltzer wrote in an email. “We can expect some transmission to occur at such locales, but hopefully on average, less than 1 person infected per infectious person.” The models show that in effective hospital quarantine, the rate of transmission is 0.12; in effective at-home, it’s 0.18; when they are not in effective isolation, it is at least 1.8.
When I spoke with Meltzer in August, he had just finished a meeting with Dr. Bryan Lewis, a computational epidemiologist at the Virginia Bioinformatics Institute (VBI) at Virginia Tech. It was an impromptu meeting in which Meltzer offered Lewis advice on the types of information aid organizations need right now. Since early July, Lewis and graduate student Caitlin Rivers have also been modeling the outbreak. (Lewis’s research funding does not cover Ebola modeling, but his funders at the National Institutes of Health gave him clearance to concentrate on Ebola, given the circumstances.) By July 18, they had a preliminary model. It is a variation on a classic model called SEIR.
The SEIR model estimates how a disease will spread through an entire population, assuming that there is normally a natural balance between death rates and birth rates within that population. It sorts people into four categories: susceptible (everyone is automatically put in this category at birth), exposed (in the case of Ebola, it can take up to 21 days for signs of infection to appear), infectious (this stage lasts an average of 3 to 15 days for fatal cases, and 10 to 25 days for recovered patients; this category includes the bodies of deceased victims) and removed (patients who have been treated successfully are considered immune). The model looks at how the sizes of the different subgroups change relative to each other.
Their model is slightly different from the CDC’s which looks at patients through five stages: susceptible, infected, incubating, infectious, and recovered.
Lewis and Rivers’s model uses 12 parameters for incubation and infectious periods, because these periods can vary so much, as well as different modes of transmission. The different modes of transmission are in the hospital setting, in the community, and in a funeral setting. To determine how many new cases are transmitted in each setting, the models require data on how people interact, who interacts enough that transmission is possible, and how many cases already exist. This data is sparse in West Africa, as is the case in many third-world areas. (Researchers studying other infectious diseases, such as dengue fever in South America, have tried putting GPS trackers on individuals in order to understand social interactions. No such project is currently underway in West Africa, as far as Meltzer or Lewis know.)
The countries impacted by this Ebola outbreak been ravaged by civil wars within the past 15 years. In Liberia, at least 350,000 people were killed in civil wars from 1989 to 1996 and1999 to 2003. In Sierra Leone, an 11-year civil war ended in 2002, with more than 50,000 dead and much of the country decimated. Guineans faced decades of military coups and misrule until 2010. These areas are still recovering, still rebuilding governments and trust, which makes it more difficult to collect data. It’s likely, according to the WHO, that cases are going unreported. Meltzer asks task-force leaders to provide as much empirical data as possible, and the CDC is currently working with local governments to standardize data collection, but for now, the CDC and VBI’s models rely on two data sources: publicly available cases over time, and historic case information regarding incubation period and length of infectious period.
Rivers also combs through local news reports and anecdotal evidence to determine how many of the new infections emerge from funerals. In West Africa it is customary for mourners to touch the body of the deceased during a funeral. Since Ebola lives on after a person has died, funeral-goers are considered at high risk for transmission. More often than not, Rivers has to input the collected data into spreadsheets by hand. Once VBI’s model for February to June started to match what the researchers already knew had happened during those months, they started to use it to project what is still to come. They run the model for the overall outbreak, as well as individually for Guinea, Sierra Leone, and Liberia, every week to predict what will happen in the coming weeks and to test the possible effects of different interventions.
The picture, as expected, is bleak. Rivers and Lewis hesitated to share actual figures from their forecasts, because the course of the outbreak could shift in ways the models cannot predict. All of their efforts, all of the modeling, can tell them what will happen if the interventions start to make an impact. The models can tell aid organizations what they need, why they need it, and when they’ll need it.
The models cannot, however, tell them how to achieve the necessary benchmarks, because there is no way to model for human behavior.
“In particular Ebola is strongly determined by human behavior, and it’s pretty impossible to predict how humans are going to start doing things. At the moment there’s a lot of resistance to some of the classic public health interventions,” Lewis said, citing the recent looting of a treatment center in Monrovia. On September 18, Reuters reported that three journalists and five health care workers were brutally killed while spreading Ebola awareness in Liberia.
“It makes a lot of sense that the population doesn’t trust authority figures, because why should they? Those are the people that burned down their villages previously. It’s going to take a longer period of time for the population to understand that the people showing up in these scary white suits are actually helping people instead of killing them.”
“The trouble is to get people to believe that going to the hospitals is in their best interest,” said Meltzer. “We’ve got to get people to understand that. You can go around to villages and cities and slums all you want and say, ‘If you’re ill, go to the hospital.’ Why should anybody believe? We can’t model that.”
They can collect empirical data from aid workers in different locations. They can see how effective a message was in one community, and see if that effect would be worth the effort in other areas, but no matter what, they can’t model human behavior.
The interventions seem to be working in Guinea, where the rate of transmission is now less than one, according to Meltzer. They have cut off the chain of the disease there, he said, and must stay vigilant in order to keep it that way. Across West Africa as a whole, though, the average transmission rate is still higher than two new infections per infectious person, according to Maia Majumder. Majumder is a Ph.D. student at MIT Engineering Systems and research fellow at HealthMap. Her group is working with an IDEA (Incidence Decay and Exponential Adjustment) model in order to estimate the growth and longevity of the outbreak, and how transmission rates change when various interventions are attempted. They are looking at some of the more recent interventions, such as closing borders and opening new treatment centers.
Their outcomes show “that what we’ve done so far has not yet been enough to make a real dent in decreasing the growth rate of the outbreak,” she said. “If nothing changes in the disease control and prevention department, case counts will continue to soar.”
It will start to subside, though, if the interventions start to make an impact. But it’s impossible to predict if the interventions will make an impact, because that depends on human behavior.
Even if the average is brought below the target of one new infection per infectious person across the entire region, though, there will still be dangerous outliers that the models do not take into account. “Some sick people won't infect anyone, and some will be super-spreaders, transmitting to perhaps a dozen people,” Rivers said. Regardless, the goal remains lowering the average rate of transmission as much as possible.
This fall, experimental Ebola vaccines are being tested in small clinical trials. Assuming the vaccination is 100 percent effective, Rivers said, “We would hypothetically need to vaccinate around 50 percent of the susceptible population to achieve herd immunity.” Herd immunity is a term epidemiologists use to say that because enough people are vaccinated, the community at large is considered immune to a disease. If herd immunity is achieved, there is a very low probability of an infected individual coming in contact with a susceptible individual. The 50 percent figure assumes that everyone interacts with everyone else. Fewer people would need to be vaccinated if they instead use the approach of ring vaccination, in which you only vaccinate people who have or will come in contact with infectious people. The ring vaccination approach was successfully used to eradicate smallpox. Lewis and Rivers are using their models to determine if a vaccine, or other new interventions, will be “just a drop in the bucket” or if they are worthwhile. According to the Associated Press, doctors are also trying blood transfusions from survivors to current patients. British nurse William Pooley will be donating blood to an American patient.
An experimental treatment called ZMapp was successfully used to treat two infected American healthcare workers, and organizations are considering whether to produce it on a mass scale. Unfortunately, Rivers explained, devoting the available funds to a large-scale production of the treatment would not be as effective as concentrating on a vaccine, because, at least historically, prevention has a bigger impact than treatment.
Even if the models show that vaccines are the way to go, though, the models will still fall short of telling aid organizations how to convince those people that getting the vaccine is in their best interest. How to make that happen can only be determined through trial and error, through trying different messages and seeing which catch on.
Right now, the most important thing aid organizations can do is to increase the percentage of patients in effective isolation settings in Liberia and Sierra Leone, according to the CDC report. (It is already considered controlled in Guinea, and has not spiraled out of control in Nigeria or Senegal.)
If they are able to increase the percentage from 10 to 13 starting today, hit 25 percent on October 23, 40 percent on November 22, and the 70-percent goal by December 22, the outbreak will peak at up to 3,408 daily cases, and will drop to less than 300 daily cases by late January.
If they don’t start increasing from 10 to 13 percent until October 23, there could be 10,646 daily cases (accounting for underreporting), and if it’s pushed back to November 22, there could be 25,847 daily cases by January 20, 2015, according to the CDC’s Ebola Response model. In that case, there could be more than 1.4 million cases of Ebola in two countries with a combined population of approximately 10.4 million people.
Even still, Meltzer, Lewis, Rivers, Majumder and other computational epidemiologists around the world are keenly aware that experimenting with computer models offers a forecast much faster than experimenting on the ground. And in the event that there is a sudden shift in public sentiment, in public trust and willingness to seek treatment, Meltzer’s model will already have told the CDC how to prepare for it.






