Amputation being performed in a hospital tent, Gettysburg . National Park Service/Wikimedia Commons
3 Plants From U.S. Civil War Medical Guide Fight Infection
A 1863 guide for battlefield surgeons reveals plants with antiseptic effects. Could they help fight drug-resistant infections today?
Three plants from a guide to traditional plant remedies of the South that the Confederate Surgeon General commissioned during the height of the Civil War have antiseptic properties, according to new research.
The results show that extracts from the plants—the white oak, the tulip poplar, and the devil’s walking stick—have antimicrobial activity against one or more of a trio of dangerous species of multi-drug-resistant bacteria associated with wound infections: Acinetobacter baumannii, Staphylococcus aureus, and Klebsiella pneumoniae.
“Our findings suggest that the use of these topical therapies may have saved some limbs, and maybe even lives, during the Civil War,” says senior author Cassandra Quave, assistant professor at the Center for the Study of Human Health and the School of Medicine’s dermatology department at Emory University.
Quave is an ethnobotanist who studies how people use plants in traditional healing practices to uncover promising candidates for new drugs. “Ethnobotany is essentially the science of survival—how people get by when limited to what’s available in their immediate environment,” she says. “The Civil War guide to plant remedies is a great example of that.”
A field hospital at Gettysburg. (Credit: National Park Service)
“Our research might one day benefit modern wound care, if we can identify which compounds are responsible for the antimicrobial activity,” says Micah Dettweiler, the first author of the paper in Scientific Reports.
If researchers can identify the active ingredients, “it is my hope that we can then [further] test these molecules in our world-renowned models of bacterial infection,” says coauthor Daniel Zurawski, chief of pathogenesis and virulence for the Wound Infections Department at the Walter Reed Army Institute of Research.
“I’ve always been a Civil War buff,” Zurawski adds. “I am also a firm believer in learning everything we can garner from the past so we can benefit now from the knowledge and wisdom of our ancestors.”
Dettweiler was still an Emory undergraduate when he heard about the Civil War plant guide and decided to research it for his honors thesis. He has since graduated with a degree in biology and now works as a research specialist in the Quave lab.
“I was surprised to learn that far more Civil War soldiers died from disease than in battle,” he says. “I was also surprised at how common amputation was as a medical treatment for an infected wound.”
About one in 13 surviving Civil War soldiers went home with one or more missing limbs, according to the American Battlefield Trust.
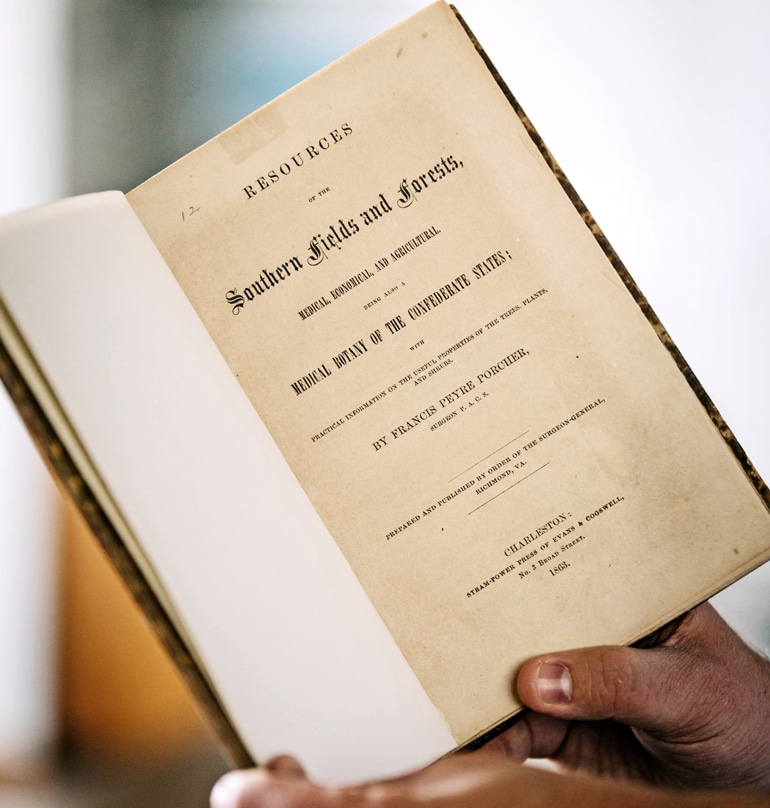
Francis Porcher, a botanist and surgeon from South Carolina, compiled Resources of the Southern Fields and Forests, which included plant remedies that Native Americans and enslaved Africans used. This 1863 copy is from the Stuart A. Rose Manuscript, Archives and Rare Book Library. (Credit: Emory)
At the time of the Civil War, from 1861 to 1865, germ theory was in its developmental stages and only gradually beginning to gain acceptance. Formal medical training for physicians was also in its infancy. An antiseptic was simply defined as a tonic used to prevent “mortification of the flesh.” Iodine and bromine were sometimes used to treat infections, according to the National Museum of Civil War Medicine, although the reason for their effectiveness was unknown.
Other conventional medicines available at the time included quinine, for treating malaria, and morphine and chloroform, to block pain.
Military field hospitals within the Confederacy, however, did not have reliable access to these medicines due to a blockade—the Union Navy closely monitored the major ports of the South to prevent the Confederacy from trading.
Seeking alternatives, the Confederacy commissioned Francis Porcher, a botanist and surgeon from South Carolina, to compile a book of medicinal plants of the Southern states, including plant remedies used by Native Americans and enslaved Africans. “Resources of the Southern Fields and Forests,” published in 1863, was a major compendium of uses for different plants, including a description of 37 species for treating gangrene and other infections. Samuel Moore, the Confederate Surgeon General, drew from Porcher’s work to produce a document called “Standard supply table of the indigenous remedies for field service and the sick in general hospitals.”
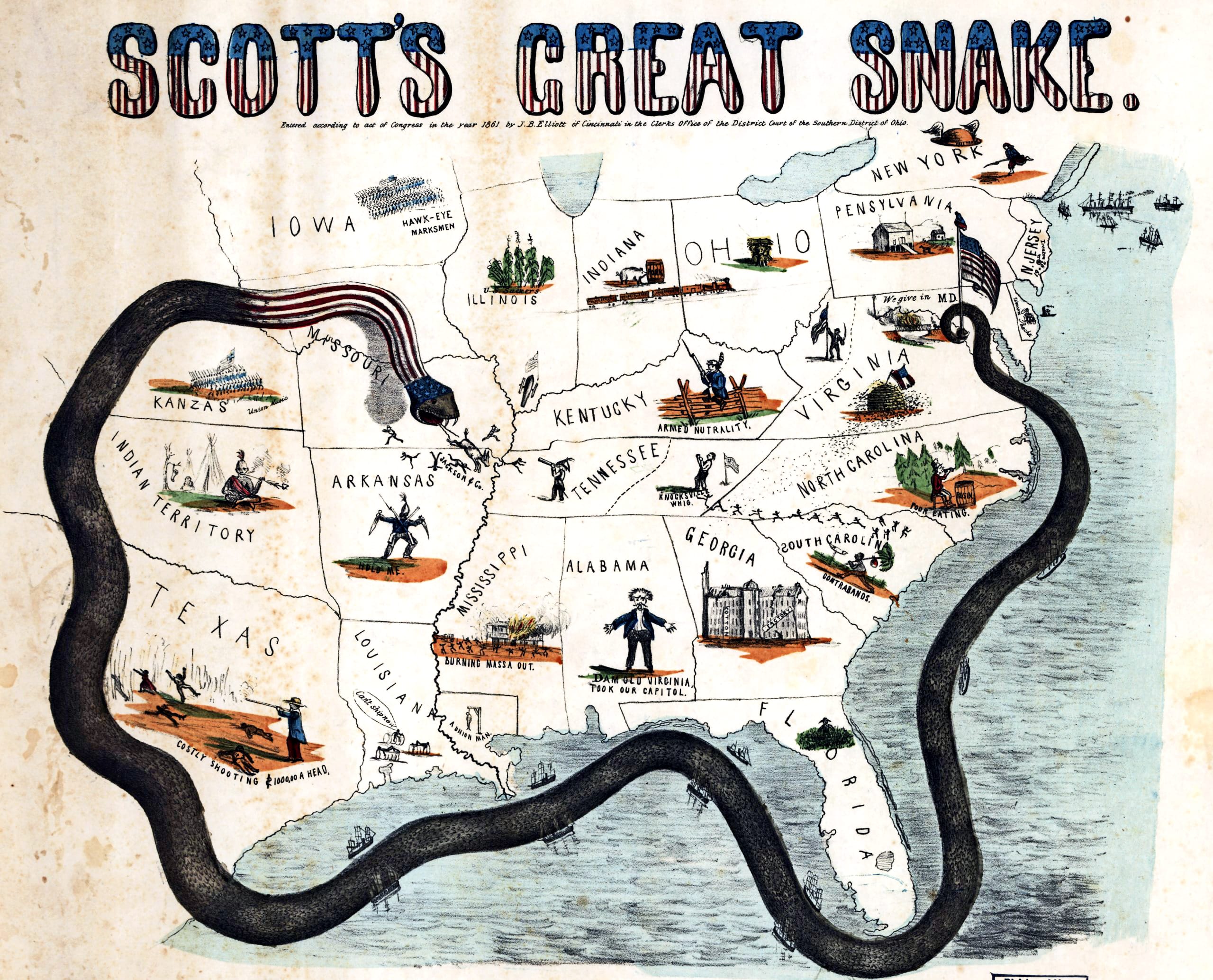
A cartoon map, created in 1861, uses a snake to illustrate Gen. Winfield Scott’s plan to crush the Confederacy economically through a blockade, sometimes called the “Anaconda plan.” (Credit: Library of Congress) View larger.
For the current study, the researchers focused on three plant species Porcher cited for antiseptic use that grow in Lullwater Preserve on the Emory campus. They included two common hardwood trees—the white oak (Quercus alba) and the tulip poplar (Liriodendron tulipifera)—as well as a thorny, woody shrub commonly known as the devil’s walking stick (Aralia spinose).
Researchers gathers samples of these three plants from campus specimens, based on Porcher’s specifications. They took the extracts from white oak bark and galls; tulip poplar leaves, root inner bark and branch bark; and the devil’s walking stick leaves. They then tested the extracts on three species of multi-drug-resistant bacteria commonly found in wound infections.
Aceinetobacter baumannii—better known as “Iraqibacter” due to its association with wounded combat troops returning from the Iraq War—exhibits extensive resistance to most first-line antibiotics. “It’s emerging as a major threat for soldiers recovering from battle wounds and for hospitals in general,” Quave says.
Staphylococcus aureus is considered the most dangerous of many common staph bacteria and can spread from skin infections or medical devices through the bloodstream and infect distant organs. Klebsiella pneumoniae is another leading cause of hospital infection and can result in life-threatening cases of pneumonia and septic shock.
Laboratory tests showed that extracts from the white oak and tulip poplar inhibited the growth of S. aureus, while the white oak extracts also inhibited the growth of A. baumannii and K. pneumoniae. Extracts from both of these plants also inhibited S. aureus from forming biofilms, which can act like a shield against antibiotics.
Extracts from the devil’s walking stick inhibited both biofilm formation and quorum sensing in S. aureus. Quorum sensing is a signaling system that staph bacteria use to manufacture toxins and ramp up virulence. Blocking this system essentially “disarms” the bacteria.
Traditional plant remedies are often dismissed if they don’t actively attack and kill pathogens, Quave notes, adding: “There are many more ways to help cure infections, and we need to focus on them in the era of drug-resistant bacteria.”
“Plants have a great wealth of chemical diversity, which is one more reason to protect natural environments,” Dettweiler says. He plans to go to graduate school with a focus on researching plants for either medical or agricultural purposes. “I’m interested in plants because, even though they don’t move from place to place, they are extremely powerful and important.”
A Howard Hughes Medical Institute Science Education Program award to Emory and grants from the National Institutes of Health, National Center for Complementary and Integrative Health, and from the National Institute of Allergy and Infectious Disease supported the study.
Source: Emory University
This article was originally published in Futurity. Edits have been made to this republication. It has been republished under the Attribution 4.0 International license.






