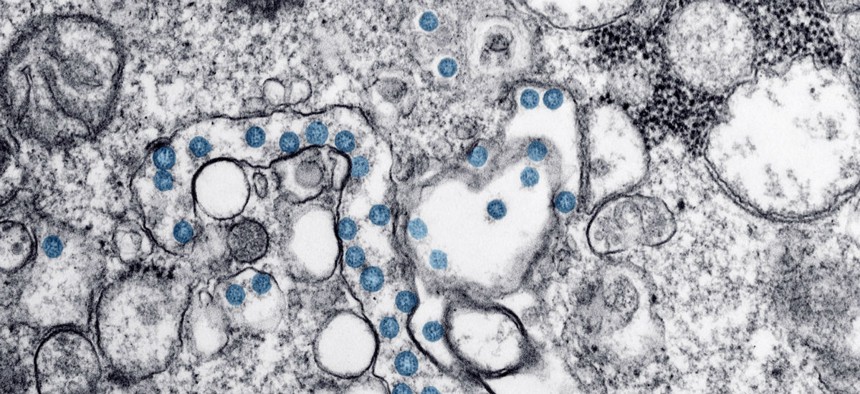
Transmission electron microscopic image of an isolate from the first U.S. case of COVID-19. CDC photo
The Four Key Reasons the U.S. Is So Behind on Coronavirus Testing
Bureaucracy, equipment shortages, an unwillingness to share, and failed leadership doomed the American response to COVID-19.
The COVID-19 outbreak has been a confusing time for Americans, but one thing has been glaringly clear: The U.S. is way behind when it comes to testing people for the coronavirus.
Despite the fact that last week, Vice President Mike Pence promised that “roughly 1.5 million tests” would soon be available, an ongoing Atlantic investigation can confirm only that 13,953 tests have been conducted nationally. New York, which has shut down Broadway and has at least 328 coronavirus cases, is still failing to test patients who have worrying symptoms. As late as March 6, a busy clinic in Brownsville, Texas, a border city of nearly 200,000 whose population crosses back and forth from Mexico frequently, told me they could only test three people. By comparison, South Korea, which has one of the largest outbreaks outside China, is testing nearly 20,000 people per day.
Testing is essential for identifying people who have been infected and for understanding the true scope of the outbreak. But when the initial test from the Centers for Disease Control and Prevention was rolled out to state public-health laboratories in early February, one of its components was discovered to be faulty. Since then, academic, clinical, and other laboratories have struggled to get or make new tests and diagnose patients.
Though some elements of the breakdown are by now understood, the full extent of the difficulties laboratory directors have faced has remained largely opaque. Interviews with laboratory directors and public-health experts reveal a Fyre-Festival-like cascade of problems that have led to a dearth of tests at a time when America desperately needs them. The issues began with onerous requirements for the labs that make the tests, continued because of arcane hurdles that prevented researchers from getting the right supplies, and extended to a White House that seemed to lack cohesion in the pandemic’s early days. Getting out lots of tests for a new disease is a major logistical and scientific challenge, but it can be pulled off with the help of highly efficient, effective government leadership. In this case, such leadership didn’t appear to exist.
Here are the four main reasons why the testing issues have been so bad:
1. Red Tape
The Food and Drug Administration has a protocol called emergency use authorization, or EUA, through which it clears tests from labs around the country for use in an outbreak. Getting more of these tests up and running would greatly increase the capacity of doctors and public-health officials to screen patients for the coronavirus.
Former FDA officials I spoke with said that during past outbreaks, EUAs could be granted in just a couple of days. But this time, the requirements for getting an EUA were so complicated that it would have taken weeks to receive one, says Alex Greninger, the assistant director of the virology division at the University of Washington Medical Center, which is located right near the heart of the American outbreak. Greninger told me clinical labs were not allowed to begin testing at all before they had received the EUA, even if they had already internally made sure their tests worked. Though these regulations are in place to ensure that faulty lab tests don’t get used on patients, several microbiologists told me they felt the precautions were excessive for a fast-moving outbreak of this scale. “The speed of this virus versus the speed of the FDA and the EUA process is mismatched,” he said.
On February 28, Greninger and dozens of other clinical microbiologists wrote a letter to Congress complaining that the EUA process was slowing down the ability of their labs to deploy coronavirus tests. “Many of our clinical laboratories have already validated [tests] that we could begin testing with tomorrow, but cannot due [to] the FDA EUA process,” they wrote. The following day, the FDA changed the EUA process so that labs like Greninger’s could begin testing—they would just have to submit data for the FDA’s authorization two weeks later. But weeks had already passed during which many labs and hospitals were unable to use their tests.
“The EUA pathway … has served for Ebola and Zika, etc.,” says Mark Miller, the chief medical officer at bioMérieux, an infectious-disease diagnostic company based in France. “And then you have a situation like now with coronavirus, which I don't think any of us have ever lived through.”
Margaret Hamburg, who served as the FDA commissioner from 2009 to 2015, told me that while she doesn’t have knowledge of what went on inside the FDA over the past few months, the agency could have proactively reached out to different national and international labs to see whether their tests could be approved for use in the U.S. For example, the FDA might ask a lab, “Would you be interested to try to redirect what you were doing for a MERS diagnostic to a novel-coronavirus diagnostic?” she says. Instead, as The New York Timesreported, federal officials told one Seattle infectious-disease expert, Helen Chu, to stop testing for the coronavirus entirely. (In an email, an FDA spokesperson denied that the agency acted slowly. Ensuring the validity of tests is important, she noted, to prevent false results.)
It looks like Chu was not alone. Dozens of labs in the U.S. were eager to make tests and willing to test patients, but they were hamstrung by regulations for most of February, even as the virus crept silently across the nation.
2. Hard-to-Get Virus Samples
Labs and companies need samples of the virus itself in order to make their tests, but delays in getting access to samples further slowed down the test-development process. The coronavirus originated in China, and as several microbiologists told me, the Chinese government does not allow specimens to be shipped outside its borders.
Many researchers have had difficulty getting their hands on samples even as the virus has spread. “I was working the phones to try to get access to the virus,” Greninger said.
BioMérieux just released three versions of its coronavirus test this week, after beginning work on it on January 23. Miller says that with every viral outbreak, the company’s biggest problem by far is getting access to virus and patient specimens so that it can validate its tests. Even when working with nonauthoritarian countries, a combination of government processes, researcher reticence, complex shipping regulations, and patient-privacy concerns makes getting samples difficult for diagnostic companies like his.
Miller said it would help if researchers, governments, and companies firmed up pathogen-sharing contracts in advance of an outbreak, but so far that hasn’t happened. “The problem is that in the past, industry has been viewed as this dirty participant in all of this, and we can't be trusted, and why would I have contracts with you?” Miller says. “But that’s ignoring the plain fact that we’re the ones that create the product in the end.”
3. Lacking Equipment
The type of test Greninger is making is called a lab-developed test. To be used in other labs, his test requires special instruments that extract and then amplify the RNA that makes up the virus. However, labs across the country—like those at many county hospitals—don’t have the tools to do this. They can only run a simple type of test called a sample-to-answer test. As late as this week, several lab directors told me that no sample-to-answer versions of the coronavirus test had been approved in the U.S. “That means that the vast majority of clinical labs in this country will not be able to do in-house testing at this time,” says Susan Butler Wu, an associate professor of clinical pathology at the University of Southern California.
The U.S. health-care system is broken up into state and county public-health laboratories, which have different equipment than academic research institutions, which have different equipment than hospitals that diagnose patients. So the same test won’t necessarily work in different places. “We don’t have a nationalized health-care system where you put the same equipment in all the hospitals,” Wu says. “We have all these independent hospital systems with their own equipment in their own labs.”
Even though some hospitals actually have the new, functional CDC tests, the extraction machines and reagents that are used to perform them are in short supply. “We’ve been pleading to the research laboratories to please, if they have RNA-extraction machines, to give them to the hospital,” says Michael Mina, an associate medical director in the department of pathology at Brigham and Women’s Hospital in Boston.
4. Leadership and Coordination Problems
For months, President Trump has made light of the coronavirus, telling attendees at a Black History Month reception, for instance, that perhaps the virus could miraculously disappear. He claimed on Twitter that the U.S. has done a “great job” handling the outbreak. Such a cavalier attitude seems unlikely to have motivated health officials to take things seriously. It also contradicted advice from most public-health experts. Even Scott Gottlieb, who recently resigned as Trump’s FDA commissioner, wrote in The Wall Street Journal on February 4 that “it’s time to start testing more people.”
Containing a new infectious disease requires a lot of close collaboration between the president, the CDC, the FDA, and other parts of the Department of Health and Human Services, several Obama-era health officials told me. “One reason we were able to move quickly [during the Ebola outbreak] was that there was a great deal of coordination and issue spotting and troubleshooting that went on,” Hamburg, the former FDA commissioner, told me.
The different arms of the sprawling health department have to feel like they’re all pulling toward the same goal. “I think you have fabulous people at CDC and FDA all doing the best they can, but we always found it was incredibly important to have all the agencies together in the same room,” says Jesse Goodman, a former FDA chief scientist who helped manage the country’s response to the 2009 H1N1 outbreak. When issues came up that merited the attention of the White House, he says, they got it.
Though Trump has proposed a payroll-tax break, as my colleague Peter Nicholas has pointed out, “Much of what he’s said publicly about the virus has been wrong, a consequence of downplaying any troubles on his watch.”
On top of that, there’s reportedly been tension and infighting between the president and his HHS secretary, Alex Azar, as well as between the FDA and the CDC. Politico reported that Vice President Mike Pence, who has no background in public health, repeatedly sidelined Azar from the coronavirus-response task force, and the White House appears to be blaming Azar for any failures in its coronavirus response. Politico also reported that an FDA scientist was “initially rebuffed”—made to wait overnight—when he attempted to visit the CDC in order to help coordinate testing. (A request for comment to HHS about these tensions was not immediately returned.)
“I gather that there was a huge amount of infighting about who could or who should lead this, and there was a sense that a lot of people [inside HHS] weren’t considering it a major threat,” said a former Obama-administration official who has been in contact with current staffers and who related these private discussions under the condition of anonymity. “And why that was, I don’t know.”
It’s possible that all of these other hurdles could have been cleared if officials at the highest levels of government had been working together smoothly. Instead, we’ve seen confusion, doubt, and even more delays.






