sponsor content What's this?

Embracing predictive data for enhanced population health
By Martin Bloomenkranz and Robert Parris
Presented by

Today, the integration of predictive, patient-level data presents a defining opportunity to elevate population health management. By shifting focus toward individualized risk assessments, healthcare organizations can unlock the potential for a more proactive and responsive approach to patient care.
Differentiating predictive and propensity data
Predictive and propensity data, though similar, serve distinct roles in healthcare. Predictive data transcends statistical probabilities based on demographics, providing an individual patient-level analysis to forecast health outcomes more accurately. Propensity data, conversely, relies on general trends and patterns to identify statistical likelihoods for population-level health risks.
Predictive data stands out for its personalized risk assessment, enabling healthcare providers to proactively deliver targeted care to people at high risk for chronic diseases like diabetes or hypertension. This data can identify who those at-risk individuals are, thereby facilitating proactive outreach, enhancing clinical outcomes, and enabling efficient care delivery.
While predictive data doesn't provide definitive answers, it can indicate discrete risk levels — beyond a mere “yes” or “no” — guiding healthcare professionals to prioritize interventions based on individual risk profiles. Beyond improved clinical care, this level of prioritization also allows healthcare systems to utilize resources more effectively. For instance, having a list of the patients at the highest risk for a particular disease or condition can help organizations better manage their response plans, tailoring appropriate levels of care to each patient based on their risk level.
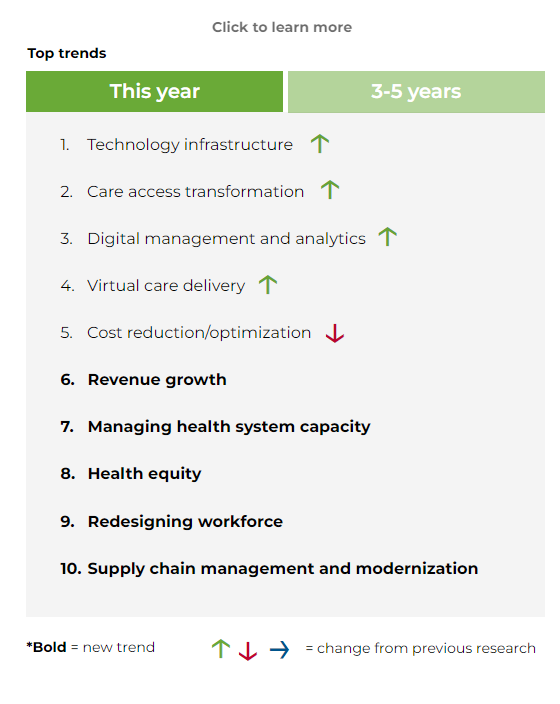
Healthcare leaders recognize the potential of predictive data analytics to make better business decisions and improve patient care. In Huron’s healthcare executive market research, leaders indicated an increased focus on technology infrastructure and digital management and analytics, as well as several other opportunities (e.g., virtual delivery, health equity, and care access) that can be positively impacted by the strategic use of predictive data.
What is top of mind for healthcare executives?
Catalyzing change through personalization
By analyzing historical claims data, demographics, and behavioral patterns, predictive data provides clinicians and administrators with actionable insights to develop targeted outreach programs that encourage preventive care and regular health monitoring. This proactive engagement has the potential to shift patients from a passive role in their healthcare to active participants, thus improving health literacy and empowerment.
Moreover, personalized care plans yield the additional benefit of enhancing the patient-provider relationship. Trust builds when patients feel that their specific needs and circumstances are understood and addressed. Predictive data enables providers to deliver customized recommendations, such as dietary changes, exercise programs, and routine screenings that better fit with patients' lifestyles. The result is often increased compliance with health recommendations, leading to better health outcomes and a reduction in hospitalizations and emergency room visits, providing needed relief to health systems’ critical high acuity care settings.
Navigating challenges for effective implementation
While the advantages of predictive data are clear, certain challenges must be navigated with care to fully harness its power. Potential misconceptions regarding the complexity of predictive analytics and its implementation can hinder healthcare professionals' acceptance and adoption of these tools. Thus, education and training initiatives for medical staff are vital. Workshops and online resources can demystify predictive data concepts, allowing healthcare professionals to see its tangible benefits in their daily practice.
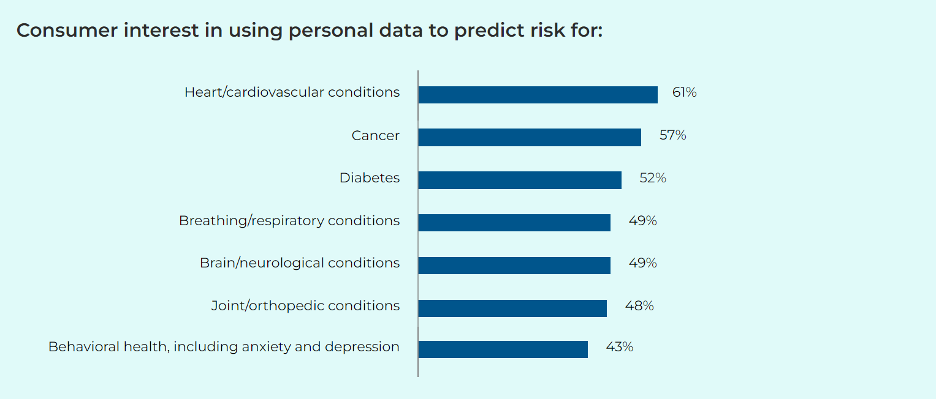
Privacy concerns are another significant consideration to address to ensure the safe, effective application of predictive data. More than half of consumers surveyed in Huron’s healthcare consumer survey indicate a willingness to share personal health data to predict risk for cancer, diabetes, and heart and other cardiovascular diseases. However, concerns about data privacy and security persist, especially when it comes to sharing genetic, mental health, and other lifestyle and behavioral information.
To address these issues, secure data practices must be employed and communicated clearly to patients. Techniques such as data tokenization, which allows health systems to be HIPAA compliant, have emerged as effective strategies to ensure sensitive information remains protected while still allowing healthcare providers to leverage essential insights gleaned from predictive analytics.
In addition, ethical considerations around predictive analytics must be closely examined. To prevent biases in predictive models that could lead to inequitable care, organizations should work to ensure diverse and representative datasets that are routinely reviewed for potential bias. By actively seeking to include different demographic groups within data, healthcare providers can better understand the unique health challenges faced by various populations.
This inclusive approach allows for more equitable intervention planning, which is critical in addressing health disparities, especially in underserved communities. Predictive data must be carefully framed in marginalized communities to address historical sensitivities and foster trust. This helps in optimal outreach and effective healthcare intervention.
The role of leadership in change management
Leadership within healthcare organizations plays a critical role in successfully adopting predictive data. Front-line clinicians, administrators, and executives must be unified in their understanding and support of predictive analytics initiatives for them to take root. Leaders must convey a compelling vision for how predictive data can enhance patient care and operational efficiency. This shared vision inspires a culture of innovation and drives the necessary buy-in across all levels of the organization.
To facilitate this transition, leaders should prioritize the establishment of supportive infrastructure for predictive data initiatives. This includes investment in technology and training as well as creating an environment that values ongoing learning and adaptability.
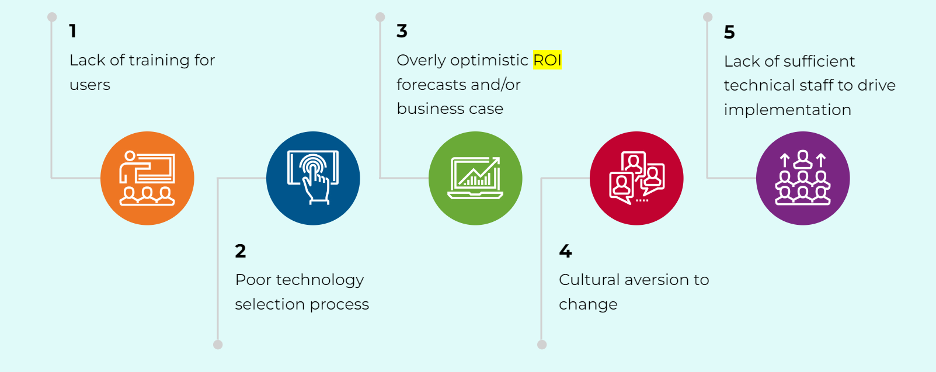
In Huron’s research, healthcare executives reported the top five reasons their digital, technology, and analytics investments don’t achieve a return on investment (ROI), one of which is “cultural aversion to change.” By promoting a culture that embraces change, healthcare organizations can effectively leverage predictive data as a catalyst for enhanced population health management.
A transformative future for population health
The proactive use of predictive data is set to reshape population health management, driving significant enhancements in patient outcomes, care delivery, and resource allocation. Emphasizing personalization alongside navigating challenges head-on will enable healthcare organizations to deliver more effective, equitable, and forward-thinking care to the populations they serve. By embracing the power of predictive analytics, healthcare providers are equipped to not only respond to current health trends but also anticipate future challenges, ultimately creating a more resilient and health-conscious society. The future of healthcare lies in our ability to harness these innovative tools and foster a culture of proactive care, ensuring each patient receives the individualized attention they deserve.
This content was made possible by our sponsor Huron; it was not written by nor does it necessarily reflect the views of GovExec's editorial staff.
NEXT STORY: GovExec TV: Five Questions with Scott Yaroschuk






